Adapted from a new final chapter that updates “The Noonday Demon: An Atlas of Depression,” to be published this week by Scribner.

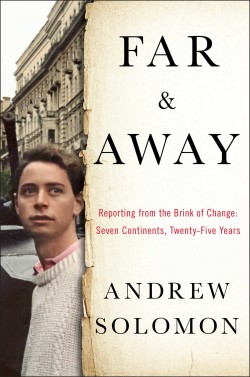
At the beginning of spring in 2013, Mary Guest, a lively, accomplished 37-year-old woman, fell in love, became pregnant and married after a short courtship. At the time, Mary taught children with behavioral problems in Portland, Ore., where she grew up. Her supervisor said that he had rarely seen a teacher with Mary’s gift for intuiting students’ needs. “Mary was a powerful person,” he wrote to her mother, Kristin. “Around Mary, one felt compassion, drive, calmness and support.”
Mary had struggled with depression for much of her life. Starting in her 20s, she would sometimes say to Kristin that she just wanted to die. “She would always follow up by saying, ‘But you don’t need to worry, Mama,’” Kristin told me. “‘I don’t have a plan, and I don’t intend to do anything.’” In recent years, Mary and her mother went for a walk once a week, and Mary would describe the difficulties she was having. She was helped somewhat by therapy and by antidepressant and antianxiety medications, which blunted her symptoms.
Mary’s friends appreciated her wacky sense of humor and her engaging wit. Colleagues said that her moods never impinged on her work; in fact, few of them knew what she was dealing with. Yet for years Mary worried that she would never be in a stable relationship and experience love or a family of her own. She said plaintively to Kristin, “I think I would be a really good mother.”
So when she discovered that she was pregnant, she was delighted, and she expected the experience to be blissful. She decided to discontinue her antidepressants, having read about their potential danger for a growing fetus. Given her history of severe depression, she was monitored closely by a psychiatric nurse practitioner, who told her that she could call anytime for an immediate prescription. But Mary elected to stay off medication.
As the months went on, she became gripped by the idea that something was wrong with the fetus, despite genetic testing and multiple ultrasounds that showed it was healthy and strong. Some nights, she spent hours online, poring over descriptions of everything that could go wrong. “We could see her spiraling downward,” Kristin said. “The really irrational obsession, the inability to see otherwise, tormented her. Her doctor tried to reassure her. But that was being rational, and rational wasn’t where she was.” One autumn day, Mary told Kristin: “I just can’t imagine being a mother.”

Mary Guest in fall 2013. Photo: Holcomb Elementary School.
By Thanksgiving, Mary, though still functioning at work, was too tired to do anything on the weekends. Her husband cared for her at home, Kristin said, and sometimes Mary would go to her parents’ house and just sit there. She was sleep-deprived because she often woke up in a panic, terrified that there was something wrong with the baby. Near the end of her fifth month of pregnancy, she finally, reluctantly, resumed taking an antidepressant.
On Dec. 9, Mary went over to sit with her mother for a while. The next day, after school, she had a therapy appointment scheduled, but she left a voice mail message, saying: “I can’t make it.” Then she went to the 16th floor of the building where her parents lived and jumped to her death, six and a half months pregnant.
“We are totally convinced that in Mary’s mind, what she did was an act of love,” Kristin told me. “That’s the only place from which Mary ever came. She was tormented that the child was going to have some serious problem, and felt it would be better not to bring this child into the world than to birth her and not be able to take care of her. We feel, rightly or wrongly, that if Mary had stayed on her medications, or even gone back on them sooner, it’s possible she would have survived.”
In 2001, I published The Noonday Demon: An Atlas of Depression, a book that tells the story of my own experience with the illness, along with those of many others, and that explores questions of resilience and of how people build their lives in the face of depression’s cruel devastation. Six years later, I became a father. I experienced anxiety around the birth of my daughter, and later that of my son — the fear of being somehow inadequate for fatherhood, the concern about losing my own stability through such a momentous change and the worry about having passed a genetic legacy of depression on to them. I also found parenthood joyous, exciting and comforting. Having children transformed my own depression, as it transformed everything else about me. I had new priorities, new concerns, new goals — but also, in some ways, a new sense of peace.
Interested in the changes that parents undergo, I pursued doctoral research and interviewed 24 women in New York over five and a half years about their experiences of motherhood. I was struck by the ways their narratives did and did not conform to mine. Even in our increasingly egalitarian society, mothers feel the weight of parenthood’s identity shift more profoundly than fathers do; they reconceive who they are, and often do so with both delight and frustration. Some of the women I spoke to had postpartum depression, and some of them were depressed before they were pregnant, while they were pregnant or both. Many were deeply ashamed of their depression. Many asked me for help making treatment decisions.
I explained repeatedly that I was not a clinician and couldn’t provide medical advice — but what these women were confronting felt like something I couldn’t turn away from. To understand the science of depression in mothers and its social implications, I ventured into the emergent field of reproductive psychiatry, reading dozens of studies and talking to experts. I found that the questions are ubiquitous, the answers sparse.
In the last two decades, it has become widely accepted that postpartum depression, which can make mothers both inattentive and irritable, is dangerous, and many states have instituted programs to screen for it and treat it. Far less recognized is an equally troubling condition: antenatal depression, or depression suffered during pregnancy, which affects up to 15 percent of expectant women. Some have been depressed for years and remain so; some have resolved previous depression with medication, go off it while pregnant and relapse; some have never been depressed until pregnancy triggers a descent into mental illness. Like postpartum depression, antenatal depression can be traumatic for mother and child. For more than half of the women who develop postpartum depression, the condition is simply an escalation of pre-existing depression; addressing the antenatal problem would ameliorate the postpartum one.
Women who felt ecstatic — or only inconvenienced — during their pregnancies may be surprised that it’s possible to have such a drastically different experience. Some women feel their best during pregnancy; others feel their worst. Averages therefore suggest that pregnancy has no significant effect on mental health — but averages don’t reveal individual experiences. Some hormonally sensitive women are predisposed to depression and anxiety triggered by puberty, menstruation, the use of fertility drugs or birth-control pills, pregnancy, childbirth and menopause. Those prone to depression at any of these times will be prone to it during the others. But that vulnerability is neither sufficient nor necessary for antenatal depression to develop; some women are depressed during one pregnancy and not the next. There are no constants.
Though antenatal and postpartum depression are linked, antenatal depression has remained underground. Much of the stigma around maternal depression — antenatal and postpartum — seems to focus on women who fail at joy, often suggesting that such women are heartless. How can anyone not be swept up by the momentousness of producing a child who will give her life purpose? The myth of the pregnant mother who is high on hormones has had considerable staying power. Something sentimental in us likes the notion that the physical discomfort of pregnancy is outweighed by the thrill of nurturing a new life within your own body. At a time of opening social mores, when mental illness is more readily acknowledged, when feminism has won women a wider range of career options, when some women’s choice not to have children is validated, when the right of gay men and lesbians to be parents has pushed the frontiers of fatherhood and motherhood, this monolithic perception of pregnancy persists. We have not acknowledged how appropriately anxiety-ridden pregnancy is, how traumatic the change in identity that accompanies prospective motherhood can be.
In dozens of interviews, I found that each woman had to invent this new identity for herself. A woman cannot know what motherhood is like until she does it — and once she does it, she cannot resign from the program. During pregnancy, she tries to understand who she will be when, as is sometimes said, a piece of her heart lives outside her body. Many mothers experience angst about the persistent admonition to expectant parents that nothing is ever going to be the same. Some imagine this vaunted change as a sentence of doom. Insofar as motherhood is a new language, it is hard to gain fluency before the child has been born. These troubling feelings are common among pregnant women, but for those with antenatal depression, they come to loom large, casting a shadow over all the positive aspects of expectancy.
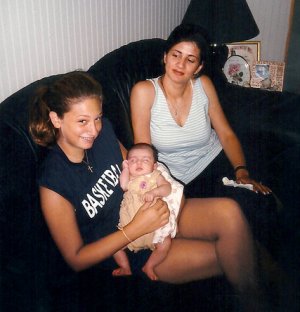
Wendy Isnardi, right, with her then-2-month-old daughter, Madison, and her cousin. Photo courtesy of Wendy Isnardi.
Many women who have endured this kind of depression speak of it in hushed voices. Wendy Isnardi was such a woman — until she decided to write a book about her experience, Nobody Told Me, and became an activist. She and I spoke numerous times by phone. She described to me suffering anxiety and obsessive-compulsive disorder during her first pregnancy, then developing acute postpartum depression. “I thought people who took medication were nuts, until I began to feel like I was really going crazy,” she said. “I had constant thoughts of harm to the baby. I knew that I was not capable of doing the things that were going on in my head, but I needed to make sure that I was not a danger.” She said she would have done anything to feel better; if she had believed heroin would help, she would have become an addict.
She now works as a counselor at the Postpartum Resource Center of New York, where she increasingly speaks to pregnant women who are unsure of how to handle their depression. Many have heard that S.S.R.I.s can be terribly harmful from online message boards, from news reports heavily influenced by an individual doctor or from small studies that have been amplified into universal statistics. The women Isnardi speaks to feel guilty about their melancholia. “They’re so afraid to be judged,” she said. “Sometimes we have to text because they are afraid their husband will overhear them on the phone.” She often refers them to support groups that welcome people with antenatal depression. “Better to be with other people who feel just as terrible as I do, and we’re all crying together,” she said.
“When you’re expecting,” Isnardi remarked, “you’re at the doctor twice a week, and nobody ever mentioned to me the possibility that I could become depressed or anxious while I was pregnant.” She was given a little care package when she left the hospital, and it contained one article about “baby blues.” She said: “If my gynecologist or obstetrician had told me there was a possibility this could happen, maybe I would have been more open to treatment while I was pregnant, and maybe it wouldn’t have gotten as bad as it did. I never even knew that was an option.”
Pregnancy is highly motivating. About a quarter of American women smoke in the three months before pregnancy, but by the last trimester only 10 percent do. This reveals how willing pregnant women are to change their behavior for the sake of the baby — and there is an increasing number of ways to do this. We have defined pregnancy as a universal Lent in which a thousand talismanic things must be forsaken for the health of the developing child. The conventional wisdom in the United States is that women should not sip half a glass of wine during pregnancy, or do the wrong kind of exercise, or take prescription medication of any kind. Some women find these relinquishments reassuring; they support an illusion that the mother’s behavior can guarantee a healthy baby. But this presumption of self-sacrifice often frightens depressed women away from seeking help.
Pregnant women with depression, especially mild to moderate antenatal depression, can often control it with talk psychotherapies such as cognitive-behavioral therapy or interpersonal therapy; almost anyone who can be helped by such interventions and who has insurance to pay for them will try them first. Some people may make use of light therapy, in which a patient is exposed to the stimulating effects of intense broad-spectrum light, though it can escalate anxiety. (For women with severe depression, ECT, or electroshock treatment, whose reputation has improved, often works, but it requires anesthesia and can provoke uterine contractions. Despite some troubling side effects, it remains one of the most effective treatments for depression in general.) Some people even turn to a selection of largely unproven devices for home use that send gentle waves of electricity into the skull. Some may use a combination; one doctor I spoke to has used cognitive-behavioral therapy to lower patients’ doses of medication while not ceasing them entirely.
Women with agonizing depression who don’t respond to other treatments, or who don’t have access to them, may take antidepressant medication. This can be dangerous for the baby. “Every woman I treat who has depression would love to be off her medication,” said Elizabeth Fitelson, the director of the women’s program in Columbia University’s department of psychiatry. “They’re taking it for a reason.”
Lee Cohen, the director of the Center for Women’s Mental Health at Massachusetts General Hospital and a professor of psychiatry at Harvard Medical School, noted: “Given women’s reluctance to take any medicine during pregnancy, the fact that so many women are using antidepressants indicates that depression during pregnancy is a real illness.”
Other doctors take much more stringent positions about prescribing antidepressants to pregnant patients. Adam Urato, an assistant professor at Tufts University School of Medicine who specializes in high-risk pregnancy, has campaigned to expose the dangers of these medications in pregnant women. On the website Common Health, he writes: “Imagine for a moment that a virus started affecting about 5 percent of all pregnant women — 200,000 U.S. pregnancies per year. Imagine that it caused significant pregnancy complications. … More than 10 percent of those infected with the virus would miscarry; up to 20 percent or more would have preterm birth, and 30 percent of newborns would show effects of the exposure in the days after birth. … It would be considered a public-health emergency. … Yet this epidemic is happening. … It is the epidemic of antidepressant drug exposure during pregnancy.” When I spoke to Urato, he compared S.S.R.I.s — selective serotonin-reuptake inhibitors, the class of drugs that includes Prozac, Zoloft and Lexapro and is the most commonly used type of antidepressant — to thalidomide, and said that their use reflected a scientific community in thrall to Big Pharma.
But while the hazards of antidepressants are real, Urato is not taking account of the whole picture. The S.S.R.I.s are among the most-studied drugs in pregnancy; the literature contains reports on more than 30,000 cases and indicates that they do not cause a clinically significant risk of major birth defects. They heighten the risk of miscarriage, preterm birth and low birth weight. They cause a slight increase in the risk of a potentially serious lung condition in newborns called persistent pulmonary hypertension. Up to 30 percent of babies exposed in utero to S.S.R.I.s develop neonatal adaptation syndrome, which entails difficulty latching on for feeding, a tremor, a weak cry, respiratory distress and sometimes reflux and sneezing, though these symptoms usually go away within a few days. There have been occasional reports of seizures and of changed sleep patterns. There have also been some gross motor delays, with exposed babies not sitting up unassisted until 16 days later than babies in a control group, though this is still within the range of normal development, and the differences have vanished by the time the children are 19 months old.
The Food and Drug Administration used a black-box warning, the strongest warning that can be attached to approved medications, to discourage S.S.R.I. use by pregnant women in 2006, at a time when the drugs were being linked to persistent pulmonary hypertension. But subsequent studies did not bear out this perceived danger, and in 2011 the black box was removed.
New research is looking at whether the drugs may have harmful longer-term consequences. S.S.R.I.s are still relatively new, so no one knows what effects exposure in utero may have on children as they grow up. Jay Gingrich, the Sackler Institute professor of clinical developmental psychobiology at Columbia, said the immediate postpartum effects of antidepressants about which clinicians such as Urato are concerned are usually insignificant. But the brain changes profoundly during fetal development and early childhood, and it changes profoundly again during adolescence and early adulthood. Gingrich, working with colleagues, exposed mice to S.S.R.I.s during the equivalent of the human third trimester of pregnancy and early infancy and found that they developed abnormalities not at the stage corresponding to human infancy but in adolescence. They showed reduced working memory, and therefore had problems with spatial tasks that mice not exposed to S.S.R.I.s solved easily.
A continuing and as yet unpublished study of mothers and children in Finland, on which Gingrich is consulting, is looking at whether these findings are echoed in adolescents exposed to S.S.R.I.s in utero. Gingrich feels there may be cause for concern. Lee Cohen of Harvard is undertaking a parallel study, hoping to chart what he calls “both the positive and negative effects” of prenatal exposure to drugs.
Ambiguity surrounds the question of medication because ethics guidelines forbid experimenting on pregnant women. You can take a group of consenting, healthy, nonpregnant women and give half of them Prozac and half a placebo, then see what happens, but you cannot do such a study with expectant women. So scientists rely on observational studies that compare women who chose to take medication while pregnant with those who didn’t. Those groups are not really parallel. Women who take medication are usually in worse shape than those who do not. I believe the ethics guidelines are sound policy: We should regulate the risks people take for themselves differently from the risks they would take for a fetus. But I also see how significantly it frustrates science.
Other studies are retrospective. If you take, for example, all children with a particular cardiac defect, check how many of their mothers took antidepressants and find a rate higher than in the general population, you might suspect that the antidepressants are causing it. But the real culprit may be maternal depression itself, or the erratic and self-destructive behaviors that often accompany it. What physicians refer to as the confounders are huge. To separate out the consequences of a depressive life from the physiological consequences of the long-term illness and from the effects of medication is nearly impossible.
Recalling the Hippocratic oath, doctors who encourage depressed pregnant women to white-knuckle it without medications for the benefit of the fetus set out to do no harm. But there can be harm not only in writing prescriptions but also in withholding them. “One of the reasons we didn’t really recognize antepartum depression for a long time was because it was easier not to, because it puts physicians in such a bind,” said Margaret Spinelli, the director of the maternal mental-health program at Columbia. Depression itself comes with its own host of problems and consequences. Learning about them, I felt hints of the despair that afflicts both doctors and patients: I was still bereft of ready answers. Those with depression may be in trouble whether they medicate or not.
Untreated depression or anxiety during pregnancy have been linked in multiple studies to miscarriage, pre-eclampsia, preterm birth, neonatal complications and smaller newborns. Antenatal depression is often accompanied by anxiety and obsessive-compulsive symptoms, and sometimes by psychosis. Cortisol, the stress hormone that is pumped up in women with anxiety and depression, crosses the placental barrier and can reach the fetus. Anxiety in pregnant women is associated with impaired blood flow in the uterine artery, which feeds the placenta.
In one study, children whose mothers were highly anxious when they were 19 weeks pregnant showed reduced gray matter at ages 6 to 9. Children of mothers who had untreated anxiety during pregnancy, other studies have found, have a higher incidence of anxiety at 4 years old, and of raised cortisol levels in adolescence.
Some scientists have reported that depression during pregnancy can alter a newborn’s amygdala, the brain region that regulates emotion, memory and decision-making, while high levels of stress during pregnancy are associated with cognitive impairment and slowed language development. Newborns of depressed mothers have been shown in one important study to have “lower motor tone and endurance” and to be “less active, less robust, more irritable and less easily soothed.” Scientists are investigating possible mechanisms through which these disturbances occur but have not yet found a clear answer.
The problems are not only biological. Women experiencing antenatal depression are more likely to engage in damaging behaviors such as drinking, smoking, drug abuse and lack of exercise. They are more likely to be obese. They often cease functioning at work, which can be financially catastrophic. They are less likely to sleep regularly or take prenatal vitamins, and they often miss obstetric appointments. Depression during pregnancy also puts an enormous strain on marriages, possibly creating a poor environment for the child.
What really struck me in listening to the physicians who treat suffering pregnant women is that while most depression is essentially private, this depression is understood to be public because it implicitly threatens others. The greatest fear among the women I met was that their depression might hurt their children. Many discounted their own suffering, even though their suffering is also part of the story. Untreated depression can take a heavy toll; this isn’t a matter just of being depressed for nine months but of a potential escalation that can result in a lifetime of struggle. The way forward may be to see the mother’s well-being and the baby’s health not as conflicting interests but as two parts of the same whole.
“I try not to draw this distinction between what’s best for the mother and what’s best for the child,” said Elizabeth Fitelson of Columbia. “I prefer to think that I’m really treating a system and trying to mitigate outcomes for the whole system, and that means that you have to pay attention to this mom’s capacity not just to bear a child but to take care of a child. The discussion is always about risk. What’s worse for the baby? Mom’s depression or the medication? Yes, that’s a very important question, but it is not the only question. Mom is suffering terribly.”
Fitelson considers, with each woman, how severe her depression has been in the past, whether she has previously tried going off medication, what other treatments have been helpful, what other measures she can try besides medication that might enable her to at least lower the dose. Fitelson also considers whether the woman has ever had an eating disorder, has a history of substance abuse, is in an abusive relationship or seems to be at risk of suicide. She asks whether the woman has other children for whom she needs to care.
Fitelson has had patients with catastrophic depression who went off their medication and then were unable to cope, to the point of terminating their pregnancies; she has also had patients whose children have deficiencies for which the mothers blame the medications they took. They all live in a penumbra of regret and guilt. “For about 10 percent of my patients, I can readily say that they don’t need medication and should go off it,” she said. “I see a lot of high-risk women. Another 20 percent absolutely have to stay on medication — people who have made a suicide attempt every time they’ve been unmedicated. For the remaining 70 percent, it’s a venture into the unknowable.”
Margaret is petite and dynamic, with an air of competent efficiency typical of many people who work in financial services. She’s warm and likable and frank, but she maintains a slight self-protective reserve when she talks about intimate subjects. (I’m using a nickname to protect her identity, as well as nicknames for her children.) Her grandmother committed suicide before Margaret was born; when Margaret was 10, her mother jumped in front of a New York City subway train and killed herself. “I have vivid memories of my mother just sitting in a chair, crying,” Margaret said. Margaret mostly held her own troubling moods at bay; when she married, she told her husband that she had a family history of depression but that she hadn’t experienced it herself.
She was working in the financial district in Lower Manhattan on Sept. 11, 2001, and though she escaped the destruction of the towers without physical injury, she began having panic attacks in which she felt as if the world around her was collapsing again. She went to see a psychiatrist who prescribed Paxil, an S.S.R.I., which calmed her down and allowed her to return to her usual life. Then she and her husband decided to have a child. She concluded, on the basis of her own research and her obstetrician’s advice, that she had to go off medication while she was pregnant. “So I came off, and I went back to being unable to function,” she recalled. “Loss of interest in things, irritability, crying, not wanting to get out of bed. Complete loss of energy or desire to do anything.”
Her baby, Katie, was colicky and strong-willed, and Margaret’s depression escalated in the months after she gave birth. She initially found it difficult to bond with Katie. “I remember saying, ‘I have so much to live for, but I can see how somebody gets to the point my mother did,’” she said. Her husband was supportive but bewildered, and Margaret worried that her short temper and disengagement would damage their marriage. When Katie was 3 months old, Margaret went on Wellbutrin and Zoloft, and within six months, she began to feel better and undertook, belatedly, the process of bonding with her child.
As Katie grew older, she was closer to her father. “I tried to be attentive when she was little, but he was the one who gave all the love,” Margaret said. When Katie was about 10 years old, she developed anxiety after an upsetting experience with food, refused to eat for a year and was nearly hospitalized for emaciation. Margaret told Katie that she herself had been afraid to leave the house after Sept. 11, that she had healed with medical support and that Katie would get better in psychotherapy. That is what happened. Margaret has worked hard to build the relationship with patient love, step by painful step.
Her first pregnancy and its aftermath were so traumatic that she waited the better part of a decade before trying to have a second child. “The first time, it was just my husband and me, so if I was in a bad mood, he would take it,” she said. “But now, knowing how strongly I want to be a great mom for my older daughter, I couldn’t have done that to her.” So this time, she told her psychiatrist that if she couldn’t have a child safely while on medication, she wouldn’t have one at all. Under his guidance, Margaret modified her antidepressant regimen. When she explained that plan to her obstetrician, the doctor was skeptical; it is not unusual for an obstetrician, who is focused on the fetus, and a psychiatrist, who is focused on the mother, to reach different conclusions. Margaret recalled telling the doctor, “This isn’t even a question for me.”
The pregnancy went beautifully: “All the things I had wanted and never got to experience with my first daughter, it was just phenomenal. I enjoyed every moment.” Her second daughter, Sally, was born healthy and strong. “She’s happy, easygoing,” Margaret said. “It was instant bonding. It was, ‘Let me rock you, hold you, giggle with you.’ And with my first daughter, it was, once my husband walked in the door: ‘Take her.’” She felt certain, she said, that it would have been a much riskier pregnancy had she not been on medication. Of course, there’s no way to know the odds. Another mother I interviewed took S.S.R.I.s during her pregnancy and has a child with multiple impairments. She said she will never forgive herself for taking medication, though she added that it helps her cope with her child’s challenges.
Margaret had felt guilt about being on medication during her second pregnancy, but now, she said, she felt guiltier about being off medication for the first one. Growing up in the shadow of two generations of family members having ended their own lives had made Margaret afraid that she might one day follow their example. She wants to protect her children from the presumption of suicide that has inflected her own episodes of mental illness. “I’ve gone to therapy, taken medication and have a great family,” she said. “I have a great job. In a way, it’s a matter of saying: ‘I’m not going to let this disease take me.’ I’m just so happy that I know it’s not going to kill me, the way I used to assume it could, and it’s not going to kill my daughters either.”
It’s clear that antenatal depression exists, but it’s not clear what should be done for it. We know too little, and none of the options are uncomplicated. But understanding some of the complexities might help millions of women who confront this condition feel less alone and make more informed decisions.
I was deeply moved by my conversations with the women whose experiences I drew on in this article, most of whom felt that their struggles had not been validated. They thought their despondent pregnancies were bizarre, outlying experiences. Some had been too ashamed to tell their husbands, their doctors, their mothers — and many of them spoke to me with evident pain when recalling what they had been through. To celebrate an experience that started in secret pain is no easy task, and mothers who had antenatal depression described how it cast a caul over motherhood.
We still have retrograde ideas about how pregnant women should feel, and we need to revise them — not only for depressed women but for all women. Pregnancy is portrayed and talked about almost exclusively as a time of rapture and fulfillment. But it involves a major shift in identity, a whole new conception of self that can lead to depression and anxiety. Change — even positive change — is stressful, and in this way pregnancy can constitute a kind of elective trauma. An abrupt transition into selflessness is not immediately appealing to everyone. Pregnant women long given to self-doubt may question their ability to take care of the child. A society that glorifies motherhood while resisting basic accommodations like guaranteed extended maternity leave makes the identity shift more frightening and abrupt than it needs to be. People given to anxiety now have a harrowing array of new anxieties to grapple with. As one woman I interviewed observed, “The things that make motherhood joyful also make it terrifying.” We should strive for a more pluralistic idea of pregnancy — for one that accommodates a wide range of moods and attitudes.
The British psychoanalyst Rozsika Parker has argued that competent mothering requires two warring impulses — to nurture the child on one hand, and to push him or her into the world on the other — and suggested that maternal ambivalence was the catalyst for achieving these apparently opposed objectives. But modern society has stigmatized the pushing and sentimentalized the clinging, and so we have denied basic truths and caused ambivalent mothers to see themselves as bad even though ambivalence can be highly productive. Mothers often exaggerate, to themselves and to others, their protective, adoring feelings, and they discount their feelings of irritation or anger as weaknesses. But a child should meet with irritation and anger some of the time; he or she should understand what those emotions are, what provokes them, how they are expressed and how they are resolved. Depression is obviously not desirable, but openness about it is tied to being honest about the challenges that motherhood entails. And that openness must begin prenatally if it is to be realized once a child has entered the picture.
There are many things that can help depressive women: the love of a supportive partner and friends, of course, but also acknowledgment of their illness and ready access to effective treatment. Most who battle antenatal or postpartum depression are committed to their children, and are trying to commit to the identity that is motherhood. For some expectant mothers and new parents, love seems to be automatic; it wafts them instantly up to a new level of consciousness. Others have to climb a very steep staircase to reach the same heights. The fact that the exercise can be agonizing and that some women cannot quite make it does not dull the intent behind it. Depression calls on resources some women have and some women don’t, including a capacity to hatch intimacy out of despair. Wanting to love your child is not the same thing as loving your child, but there is a lot of love even in the wanting.
Paula Modersohn-Becker, Reclining Mother and Child, 1898.